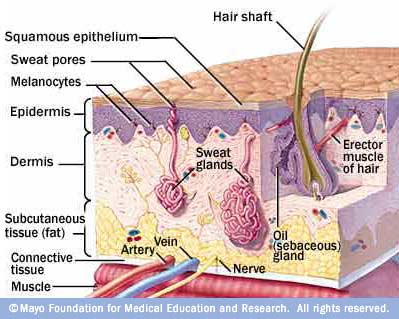
Skin is the largest organ of the human body, represents about 16% of the total body weight, and covers the large majority of the body. As the external covering of the body, skin is the first line of defense against infection from pathogens in the environment. Skin also provides the sensation of touch and pressure, prevents water loss, insulates the body, and regulates body temperature. Therefore, it is an essential barrier and mediator to the outside world that must be maintained. Primary methods to restore irreversibly damaged skin include skin grafts and transplants.
Skin grafting is a step on the reconstructive ladder for wounds that cannot be closed primarily. The "reconstructive ladder" is a generalized term coined to describe complex stepwise procedure to treat physical external injury. Skin grafting is categorized into five distinct types: Autologous (donor and recipient are the same), Isogeneic (donor and recipient are genetically identical), Allogeneic (donor and recipient are same species), xenogeneic (donor and recipient are of different species), and prosthetic (replacement of lost tissue by synthetic materials).
Thursday, December 3, 2009
Conclusion
First the wound is prepared by revascularization of the recipient bed and homeostasis. The recipient bed must be completely clean (no bacteria) as well. Next the graft is meshed (short, uninterrupted cuts) in order to prevent fluid accumulation under the graft, to stretch over a larger area, and to accommodate the shape of the targeted area. The graft is then placed on the prepared wound bed and attached with surgical staples or stitched on. Often bolster dressings and negative pressure dressings are applied with sutures to keep light, yet firm pressure on the graft and prevent fluid collection between the graft and the bed. Negative pressure dressings places foam over the graft, The success of skin grafting is dependent on nutrient uptake and vascular ingrowth from the recipient bed, which occurs in 3 phases. The first phase occurs in the first 24-48 hours where the graft is attached to the bed with a fibrin layer and a diffusion of nutrients is initiated (plasmatic imbition and the transfer of nutrients from the bed to the graft). The second phase happens in the next few days when a vascular network is established and donor and recipient capillaries are alligned (inosculation). By seven days, the third phase of revascularization and new vascularizationis achieved. If all goes well, by 2-4 weeks, reinnervation has occurred (growth of nerve fibers from the bed into the graft).
While a skin graft is often a successful surgery, there are various risks and dangers than can arise. Obviously, bleeding is a result of any surgery, as well as infection and scarring. Skin grafting can also lead to loss of sensitivity and sensation in the skin, a constant pain, and cosmetic issues such as discoloration. Although skin grafts are an effective way to treat burns, there are complications that inhibit their efficacy. Firstly, the patient’s body might reject the skin graft used on the wound. Human leukocyte antigens prevent skin graft transplantation from one individual to another. Since five linked genes, each with multiple alleles at each locus, determine the HLA group, it is very difficult to find matches among individuals. Another complication is the healing time of the wound. If left to heal naturally, it may take months for the skin to epithelialize and merge with the graft. Adding moisture artificially to the wound via Non-Contact Normothermic Wound Treatment only exacerbates the problem because it causes exudate, a protein that triggers inflammatory cells, which retards the healing process.
These complications have led to high cost for a skin graft surgery. The immunosuppressants that many patients take are expensive and are required for a lifetime. More importantly, the time required to stay in the hospital places a large cost burden on the current healthcare system. In addition, some people question if this technology is being used efficiently when the surgery is purely cosmetic and maybe not necessary. Certain surgeries should not be done as they are strictly for cosmetic purposes and sometimes the victim is just looking for a large lawsuit (i.e. Liebeck vs. McDonalds). While the Tort Reform will help prevent this, this can be a major problem of skin grafting in the current healthcare system.
As a method that has been in existence since 2500 B.C., skin grafting is clearly vital to the survival of many patients. A perfect example of this is the story of Michael Brewer. Having eighty percent of his body burned, his only choice for survival was skin grafting. Doctors say his recovery will keep him in the hospital for a long time, possibly a year or two. While this cost will be massive for the healthcare system, it is the only way Brewer could survive. Its importance is not the only reason for its sustainability. Recent technology innovations have the potential to take burn and wound victims like Brewer and speed their recovery to as quickly as three weeks. Recent discoveries in burn vacuums, stem cells, and nanotechnology are shedding light on the new possibilities of skin grafting. The spray-on skin cell technology has cut hospital stays for some victims from twenty-one to five days, which is incredible since each day can cost nearly $4000. These new technologies will keep skin grafting around as they will not only improve the lives of patients but also reduce the costs necessary to keep the patient alive and healthy.
New research at Johns Hopkins has shown that not only HLA tissue typing is essential for the success of skin grafts, but also platelets (the small cells that circulate in the bloodstream that help clotting). Similarly, recent developments such as negative pressure wound therapy (NPWT) have allowed huge strides to be made in the efficiency, cost, and success of skin grafts and transplants. As mentioned before, spray-on skin cells have been noted as a possible area for improvement in the treatment of burns and nanotechnology as well. Although biotechnological innovation for skin grafts is expensive, there is a a huge realm of possibility for improvement in terms of the effectiveness of the graft (preventing infection and other post-surgical complications) which will reduce in-hospital stays. Therefore, further research is required in order to achieve better and less expensive treatments for wounds that cannot be closed primarily.
History of Skin Grafts
As we continue to discuss current skin grafting techniques and where this biotechnology is headed, this is a short article discussing where it came from and how old it is.
Monday, November 23, 2009
Spray-On Skin Cells
The other posts this week wanted me to find an article dealing with a different field of skin transplants, which is how I came across this National Geographic article. This article was written in 2005, which is when this potential technology was first being discovered. "When burns extend over 50 or 60 percent of the body, patients don't have enough of their own skin to cover them." The process will help severely burned patients to faster and better recovery.
 http://www.technologyreview.com/biomedicine/23876/
http://www.technologyreview.com/biomedicine/23876/The technique involves taking a small patch of the patient's healthy skin cells and growing them in a lab to then be sprayed on the patient. Since this technology is still undergoing development, its full potential is still not known. The article discusses research trials being done to test the spray-on skin cells ability to fill in the holes of normal skin grafts. The research was testing whether burn victims that were then treated with the spray-on skin recovered faster than just normal skin grafts. While I am having difficultly finding the results of this research, the importance of this development was expressed in this article.
"The average hospital stay for a burn victim can cost up to $3,680 (U.S.) per day and can last for about two weeks. In contrast, a single spray treatment can cost about $9,000 (U.S.)." This financial advantage is just one positive to the new technology. It has also been shown that the faster recovery for the burn victims helps to reduce the severity of the scar tissue.
More research into this new biotechnology innovation led to some other interesting concepts that could possibly develop. One creative innovation would be a "spray-on gun," which is quickly discussed in the link below. This would allow skin cells to instantly be applied to wounds, such as for soldiers that undergo battle wounds. The following link is about Dr. Fiona Wood (Dr. Fiona Wood), the doctor that discovered this innovation. The article is worth reading to see how important her research is:
"Following her work done for victims of the terrorist attack in Bali, Dr Fiona Wood's unique solution for burns victims has attracted worldwide acclaim. Currently Director of the West Australian Burns Service and co-founder/Director of Clinical Cell Culture Ltd, this pioneering doctor's technique known as 'spray-on skin,' helped to substantially reduce the death toll of the Bali bombings. Wood's method allows for the rapid administration of skin cells, speeding up the healing process and significantly reducing scarring. Where previous techniques of skin culturing required 21 days to produce enough cells to cover major burns, Wood's innovative technique has cut this time to 5 days. "
Spray-On Skin Cell Gun
Nanotechnology and Skin Grafts
Last week the majority of the articles we posted dealt with how
skin grafts work and the different options of skin graft therapy
available to the patient. However, this process takes months and
years to heal and get the patient up to a functional state. So I
investigated methods in which the process can be expedited. Are there
any ways to speed the process? This week I focused on treatment of
severe burns using a combination of different fields. This article,
written in October 29th in 2009 deals with the use of nanotechnology
in order to accelerate the healing of skin grafts and burn wounds.
This is an excerpt from the article:
"The repair and management of extensive burn wounds have long
been a problem and served as a difficulty in conventional Tissue
Engineering methods. Autografts are often used in burn treatment;
however, insufficient supply and the secondary wounds created from
harvesting autografts limit its applicability for extensive burns.
Autologous tissue engineered skin substitutes (ATESS) are considered a
promising alternative to autografts. They possess many of the
properties of an autograft, such as wound protection, accelerated
wound closure, high graft take, new skin regeneration, and not subject
to immunorejection. For extensive burn treatment using ATESS, there
are two unsolved and critical issues: 1) the in vitro time to create
the skin substitutes should be as short as possible, allowing rapid
wound closure; 2) the size of ATESS should be as large as possible to
cover enough wounded area. Current tissue-engineering approaches
require prolonged culture time and cannot produce large skin
substitutes. Therefore, it is desirable to develop new approaches and
strategies toward rapid production of autologous skin substitutes with
up-scaling potential. The primary objective of our research is to
develop a novel practical protocol for rapid creation of ATESS using a
nanofiber-enabled layer-by-layer cell assembly approach. Our specific
aims are: 1) in vitro preparation and characterization of skin
substitutes using layer-by-layer assembly of skin cells, 2) in vivo
determination of the effect of tissue engineered skin substitutes on
the healing of acute full-thickness wounds in a mouse model."
Of course, this is a new frontier in skin graft treatment, but
the prospect of using nano- scaffolds to speed the grafting of skin to
the wound is more than hopeful, it is tangible.
The Use of Stem Cells for Burn Patients?
Stem cells could create new skin to help burns victims
New research shows that human embryonic stem cells can be used to create new skin, which can then be used for serious burn victims. So far research has only been done on mice. Research has shown that stem cells grew into fully formed human skin 12 weeks after being grafted on to mice. This progress could result in a number of advantages for the skin graft procedure. Advancements with stem cells could result in solving problems with rejection and risk of dehydration and infection.
Most often, a patient suffering from a serious burn normally have a technique where new skin is grown in the laboratory from the patient’s own skin cells, which is then grafted on to the affected area. This technique take about 3 weeks, which leaves the patient at risk of dehydration and infection. Usually skin from a cadaver is used to cover the area that the skin is taken from, however it is not always available and could potentially be rejected.
This research could potentially lead to "an unlimited resource for temporary skin replacement in patients with large burns awaiting grafts of their own skin", with a much smaller risk of rejection. This could lead to a number of advancements in skin grafts, which could even not only more efficient and less painful for the patient, but potentially more cost effective.
There may be one issue from this research. This is due to the use of human embryonic stem cells. The public opinion would be very important, and some may be concerned about the ethical issues surrounding this. Some believe that the embryonic stem cells are a source of life, and therefore by using the stem cells potential life is being destroyed.
It will be interesting to follow this research. The procedure has only been tested on mice, and now needs to go through human trials. I am interested to see if the procedure works similarly as effective or differently to that of the mice. Assuming it succeeds it could develop many advantages to the world of skin grafts.Sunday, November 22, 2009
Xenograft Rejection Inhibition
There are numerous types of skin grafts and so far, this blog has discussed different applications for some of these grafts. One type of graft that has not been discussed are xenografts. Similar to most transplants, xenografts often result in rejection. This article discusses a possible method for the inhibition of skin xenograft rejection. Xenografts are often used as temporary skin transplant recipients, such as burn victims, until a proper allograft transplant can be done. The experiment's basic test was to compare the effects of altering T-cell receptors in mice on how long rat grafts survived in the mice. Overall, the experiment had positive results as one variation in the alteration of the T-cell receptor allowed a rat graft in a mouse was able to survive fifty-four days compared to the standard nine. While the experiment does not discuss potential applications for humans (such as a porcine xenograft being used for a burn victim), this study and article shows that there is potential uses for xenografts even though they generally end in rejection by the host body. The use of xenografts is important to current health care debates because allogeneic transplants are not always available when a patient is in desperate need for one (even though this occurs more with other organs than with skin).
Leg Ulcers

Skin Grafting for Diabetics
I looked for an article dealing with diabetic leg ulcers since both my dad has diabetes and my grandfather passed away from complications of the disease. Foot ulcers was a large complication that my grandfather had to battle and it unfortunately led to several amputations. This article discusses an important use of skin grafting for diabetics with leg or foot ulcers. Ten to fifteen percent of diabetics are at risk of this danger, which is the leading cause of hospitalization and amputation. While the current treatment of wound wraps and protective footwear can be successful, it is inefficient at healing all ulcers. This article, which was published in the late 90s when the method was first being tested, details how successful skin grafting can be for diabetics. The skin grafting method provides diabetics with an alternative to the lengthy time and money that may need to be spent for hospitalization or amputation.
Saturday, November 21, 2009
Graft Rejection
Platelet Rejection: http://www.sciencedaily.com/releases/2009/02/090217173038.htm
Picture: http://www.pennmedicine.org/health_info/images/19192.jpg
These are the current theories on graft rejection.
Monday, November 16, 2009
Burn Vacuum
My second article deals with a solution to the medical predicament discussed in Non-Contact Normothermic Wound Treatment. This video shows a teenage boy who suffered second and third degree burns all over his body from a gasoline burn and required skin grafts to heal his wounds. A doctor by the name of Joseph Molner is using a special vacuum on his patient’s wounds to suck out the moisture and impeding the growth of exudates and inflammatory cells. This vacuum not only speeds up the healing process but also allows for the grafts to epithelialize to the skin at a much faster pace as well. From my research, I was amazed by the seemly contradictory treatments that both work on healing wounds, but different kinds. To treat chronic wounds, moisture and heat must be added to promote epithelization of the skin grafts and the skin attached to it. This summons immune cells to fight off bacteria and creates an environment to hot for bacteria to thrive. However, if the patient suffers from acute wounds and requires split thickness skin grafts, excess heat and moisture exacerbates the epithelialization of graft and skin. Thus, moisture must be removed from the wound to stop the build up of exudates and inflammatory cells that impedes healing.
Non-Contact Normothermic Wound Treatment
Picture: http://www.woundsresearch.com/files/wounds/imagecache/normal/photos/gouldfig1.jpg
My purpose for this week was to find articles that reflected the
possible complications associated with skin grafts. In particular, I
ascertained the possible problems of efficacy in the NNWT (Non-Contact
Normothermic Wound Treatment) of severe wounds. This kind of
treatment involves a device stationed in close proximity to the wound
and the application of heat to the area in order to induce immune
cells and kill bacteria, among other effects. The controversy of this
treatment is whether NNWT is efficacious for treating acute wounds in
addition to chronic wounds. The first article deals with an
experiment conducted to see if NNWT is indeed efficacious in treating
Split Thickness Skin Grafts. The results proved that NNWT does not
heal STSG as well as chronic skin grafts because the added moisture
produced on the wound by the heat in NNWT caused exudates a protein
that triggers inflammatory cells and thus retards the healing process.
As such, it is better to find a way to decrease such moisture so that
the skin and the grafts attached to it can epithelialize properly, but
NNWT clearly does not achieve this.
Liebeck v. McDonalds
Legal Myths: The McDonald's "Hot Coffee" Case
More Info on Tort Reform (blog)Obama on Tort Reform (CBS transcript)
NYT articles on Tort Reform (malpractice)
This case involves a 79 year old Stella Liebeck in New Mexico who in 1992, bought a cup of coffee at a McDonalds drive-through and spilled it on herself (coffee at about 180-190 degrees Fahrenheit). She incurred 3rd degree burns, and underwent skin graft operations (hospitalized for about a week). After denied attempts to settle with McDonalds for hospital costs, Liebeck took the case to court and was awarded "$2.9 million" in damages which was later reduced (however the headline stayed).
I thought that this article dealt more with the health care debate side of skin grafts (albeit in a slightly separated yet interconnected way). This case has since become one of the cornerstones concerning the debate over "excessive lawsuits". Tort Reform is a collection of proposed reforms that "all are designed to either limit the circumstances under which injured people may sue, limit how much money juries may award to injured people, or both" (whatistortreform.com). Tort reform is one method of reform that many (politically, mostly Republicans) think is the best way to reduce medical malpractice suits.
This article is found on a medical website, and was written by a doctor. The information provided is the basic information about skin grafts. It is not overwhelming with specific details and gives the impression that most of the time skin grafts are quite successful. Without prior knowledge of skin grafts, this site is very helpful in getting one started.
Brave New Face
Brave New Face
picture: http://www.newscientist.com/data/images/ns/cms/dn9010/dn9010-1_650.jpg
In researching skin grafts, I thought it was important to begin to look at the different types of grafts. An area that is beginning to gain more attention is the area of face transplants. One of the first partial face transplants took place in France after an awful dog bite. This article is looking at the considerations in planning a full facial transplant.
This procedure is very complicated and difficult. Not only does the skin need to be considered in terms of the HLA’s (Human Leukocyte Antigens) but it also needs to be considered in terms of skin tone, age of the donor, and the sex of the donor. It is much more complicated than your normal organ transplant. The procedure in total can take a long time, almost 15 hours, and the transplantation is difficult due to the large number of nerves in the face. Success in a facial transplantation relies on the growth and healing of the nerves in the face, which cannot be evaluated till about nine months after the procedure. Depending on how well these nerves heal impacts how well the patient maintains mobility in their face in the long term after the procedure.
This article also raises the question of the emotional impacts of a procedure like a full facial transplant. For example, a full facial transplant would result in someone else’s face being put on the patient’s face. This could potentially be very traumatic for the patient, and difficult to deal with. The procedure is psychologically difficult, not only for the patient, but also for the family. It may be difficult for the family to see a different face on their loved one. The idea is that in time the patient will eventually be able to recognize and identify with their new face as if it is their own.
Along with this the patients runs the risk of the transplant being rejected. It is also probable that any patient that undergoes a complete face transplant would be overwhelmed by media attention. This could be very stressful for the patient.
The research that this doctor is doing before this procedure is very extensive, and involves more than just skin tone, and age, but also the best way in which the skin can be attached to as effectively as possible provide mobility to the face, especially around the ears and lips, which in the past have yielded poor results.
In terms of health care, this type of procedure could be interesting, as the length of the actual procedure and the immunosuppressant drugs following the procedure may make this a potentially expensive procedure. It could be interesting to see the involvement of insurance companies or government aid in a procedure like this, even if it is a more rare procedure.
I am interested to find out if this procedure ever was completed, seeing as the article was published in 2006, and if so, if the procedure was successful.
Skin Graft - Medicine Plus
Skin Graft- Medline Plus
picture: http://ebsco.smartimagebase.com/imagescooked/9149W.jpg
Skin grafts and transplants are a crucial surgical development in biotechnology. This is especially utilized with burn victims. This website contains some basic information in understanding the procedure of a skin graft, the different types, risks of the procedure, reasons it is used, and post-operative care. For anyone searching for basic information, this site is very helpful.
A skin graft involves removing a patch of skin from one area and attaching it to a wounded part of the body, where skin needs to be regenerated. There are two basic forms of a skin graft: split-thickness skin graft and a full-thickness skin graft. Most of the time patients undergo a split-thickness skin graft, which takes the top two layers of skin from the donor site. With more serious wounds, that have deeper tissue loss, a full-thickness graft is used which removes the entire thickness of the skin, including muscles and the blood supply. It is incredible that this is possible, including the re-growth of blood vessels.
Skin, Grafts: eMedicine Plastic Surgery
Skin, Grafts: eMedicine Plastic Surgery
Picture: https://www.bcbsri.com/BCBSRIWeb/images/image_popup/skin_type.jpg
This article details the basic anatomy regarding skin grafts, the types of skin grafts, operative technique, success rate of skin grafts, and finally biologic skin substitutes. The information establishes our foundation of knowledge about general biological background of skin grafts, how skin grafts work, and alternative methods of skin grafts (other than the basic autogenous graft).